Standing up should be simple. But for people with Postural Orthostatic Tachycardia Syndrome (POTS), it can feel like climbing a mountain. Dizziness, a racing heart, and crippling fatigue turn daily tasks into battles.
If POTS turns your life upside down, you might wonder: Is it a disability? The answer lies in how it reshapes lives. While not life-threatening, POTS can strip away independence, making work, school, or even grocery shopping feel impossible.
Let’s break down the facts.
POTS: More Than Just Dizziness!
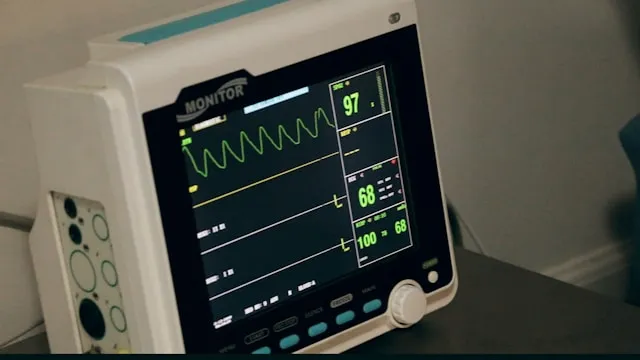
POTS is a blood circulation disorder. When you stand, your heart races to compensate for poor blood flow to the brain. Adults see a 30+ bpm spike; teens hit 40+ bpm within 10 minutes of standing. It’s not anxiety or dehydration—it’s a malfunction in the autonomic nervous system.
Symptoms vary. Some feel lightheaded. Others battle fatigue, brain fog, or nausea. For the remaining people, symptoms are debilitating enough to disrupt work, school, or social life. This raises the question of whether POTS is a disability. Well, the answer depends on severity.
Is POTS a Disability? Legal and Practical Perspectives
In the U.S., disabilities are defined by the Americans with Disabilities Act (ADA). A condition qualifies if it “substantially limits major life activities.” For POTS patients, standing, walking, or even thinking clearly can become impossible.
When POTS Meets Disability Criteria:
-
Work Limitations: Jobs requiring prolonged standing (e.g., teaching, retail) may become untenable.
-
Daily Challenges: Tasks like cooking or shopping may require assistance.
-
Health Care Costs: Frequent doctor visits and medications strain finances.
|
Disability Benefits Eligibility |
Requirements |
|
Social Security Disability (SSDI) |
Proof that POTS prevents full-time work for 12+ months. |
|
Workplace Accommodations (ADA) |
Flexible hours, seated work options, or remote arrangements. |
Not everyone with POTS qualifies. Documentation from cardiologists or neurologists is critical. Case reviews show approvals often depend on symptom severity and functional limits.
Who Gets POTS? Risk Factors & Causes
POTS doesn’t discriminate by age but favors women. Studies estimate 1 to 3 million adults and children in the U.S. live with it. Most are women aged 15-50. Up to 75% develop POTS after viral infections (e.g., COVID-19), surgery, or trauma.
Risk factors include:
-
Family history of autonomic disorders
-
Hypermobility syndromes (e.g., Ehlers-Danlos)
-
Autoimmune conditions like lupus
Symptoms That Redefine Daily Life
POTS isn’t just a fast heartbeat. It’s a cascade of issues:
-
Physical: Standing triggers fainting, tremors, or migraines. Simple acts like showering or cooking become risks.
-
Cognitive: “Brain fog” blurs focus—forgetting words mid-sentence or zoning out during conversations.
-
Emotional: Isolation grows as plans get canceled last minute. Fear of collapsing breeds anxiety.
Heat waves skipped meals, or stress crank symptoms higher. Imagine mapping every errand around rest breaks or cool spaces. For many, this isn’t choice—it’s survival. When survival eats your time, is POTS a disability? For those bedbound or jobless, the answer tilts yes.
Treatment: Can You Manage POTS?
Living with POTS means finding a mix of fixes that work for your body. No single fix cures it, but many tools can help you cope. Here’s what works—and what doesn’t.
1. Diet: Salt, Hydration & Eating Strategies
-
Salt Up: Aim for 8-10 grams of salt daily. Sprinkle it on food, drink broth, or take salt tablets. Salt holds water in your blood, which stops your heart from racing when you stand.
-
Hydrate Hard: Drink 2-3 liters of fluids a day. Water is key, but electrolyte drinks (like sports drinks) add minerals lost through sweat or pee.
-
Eat Small: Big meals pull blood to your gut. Eat 5-6 small meals to dodge crashes. Avoid alcohol—it dries you out and worsens dizziness.
2. Exercise: Slow and Steady Wins
-
Start Low: Lie down or sit for workouts. Try recumbent bikes, rowing machines, or swimming. These keep blood from pooling in your legs.
-
Build Step by Step: Add 1-2 minutes to workouts each week. Push too fast, and you’ll crash. Stop if your heart races or you feel faint.
-
PT Help: A physical therapist can design a plan. They’ll teach moves to boost leg strength and train your body to handle standing.
3. Meds: Tools, Not Cures
-
Beta-Blockers: Slows a racing heart. Works best if your pulse spikes over 120 when standing.
-
Midodrine: Squeezes blood vessels to push blood upward. Take it 3x daily, but don’t lie flat after—it can spike blood pressure.
-
Fludrocortisone: Helps kidneys hold salt and water. Good for those with low blood volume.
4. Gear: Small Tools, Big Relief
-
Compression Wear: Waist-high stockings (20-30 mmHg pressure) stop blood from pooling in the legs. Wear them daily.
-
Cooling Vests: Heat worsens POTS. A vest with ice packs lets you go outside in summer.
-
Shower Stool: Sitting stops faints during hot showers.
Warning Signs: When POTS Becomes an Emergency
On most days, POTS is manageable. But some symptoms need quick care:
-
Chest Pain: Sharp or crushing pain could signal heart issues—not just POTS.
-
Fainting with Injury: Hit your head? Get checked for concussions.
-
Can’t Keep Fluids Down: Vomiting for 12+ hours? IV fluids may save you from collapse.
-
Sudden Weakness: If one side goes numb or speech slurs, rule out stroke.
Final Thoughts: Is POTS a Disability Worth Fighting For?
POTS can be a disability—not by label, but by lived experience. When standing steals your breath or work feels out of reach, the law may back you. Document every symptom. Track how tasks crumble. Use that data to fight for benefits or job changes.
But beyond laws, POTS demands grit. Small steps—extra salt, therapy, a shower stool—add up. Lean on communities who get it. Share your story; shame dies in sunlight.
If POTS hijacks your life, consult a specialist. Push for tests. Demand trials of meds. You deserve more than survival mode.
Think POTS limits you? Talk to a cardiologist or neurologist now. And share this post—someone you know might be fighting in silence.
Frequently Asked Questions
Does POTS shorten lifespan?
No. It impacts quality, not longevity. Risks come from falls or delays in care.
Can diet alone fix POTS?
Rarely. Most need meds + diet + exercise. Salt helps, but isn’t a cure.
Is exercise safe with POTS?
Yes, if paced. Start horizontal (rowing, swimming). Skip upright workouts early on.
Can POTS affect grades?
Yes. Brain fog disrupts focus. Seek school plans (IEPs/504s) for extra time or breaks.
Is POTS considered autoimmune?
Sometimes. Research links some cases to autoimmune issues, but available proofs are young.
Do symptoms ever fade?
Maybe. Teens often improve; adults see slower progress. Remission is rare but possible.
Reviewed by